Plasma Exchange Plasmapheresis Overview and Procedure
Therapeutic plasma exchange is a physician-directed medical procedure that focuses on altering the composition of a patient’s plasma. Plasma is the liquid portion of blood that carries proteins, antibodies, and signaling molecules throughout the body. In certain medical conditions, some of these circulating components can contribute to inflammation, immune dysfunction, or disease progression.
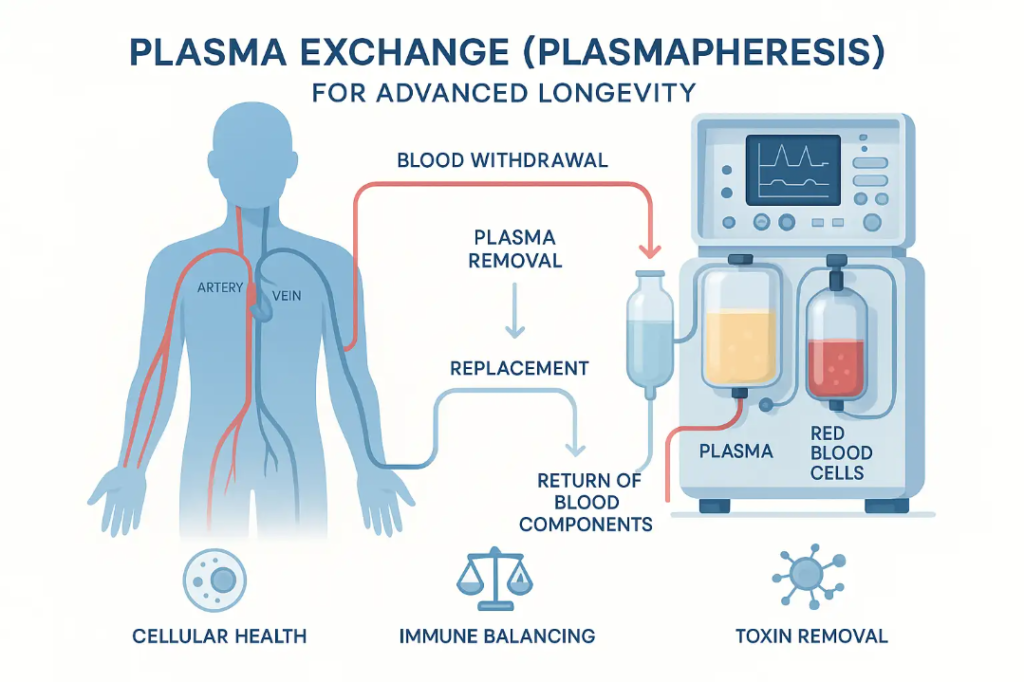
During therapeutic plasma exchange plasmapheresis, plasma is separated from blood cells and removed. The blood cells are then returned to the patient along with approved replacement fluids. This process allows clinicians to reduce the concentration of specific plasma-based substances while maintaining normal blood cell function. Therapeutic plasma exchange is most commonly used in hospital or specialty apheresis settings for defined medical indications.
At Thrive Medicine Clinic in Houston, Texas, patients may also learn about plasma-based therapies such as Young Plasma Exchange, which involves the intravenous administration of donor plasma under medical supervision. This service is distinct from hospital-based therapeutic plasma exchange and is offered within a wellness and regenerative medicine context following consultation and screening.
How Plasma Exchange and Plasmapheresis Work
Plasmapheresis is the technical process used to separate plasma from blood cells. Specialized medical equipment draws blood through an intravenous line and directs it into an apheresis device. Using centrifugation or membrane filtration, the device separates plasma from red and white blood cells and platelets.
Once separation occurs, the blood cells are returned to the patient. The removed plasma may be discarded or replaced depending on the clinical purpose of the procedure. Replacement fluids can include saline, albumin, or donor plasma, selected by physicians based on medical indication, laboratory findings, and patient health status.
Throughout the process, vital signs and blood parameters are monitored to maintain circulatory stability. These controls help ensure that plasma exchange is performed in a consistent and medically appropriate manner.
Therapeutic Applications and Medical Use Cases
Therapeutic plasma exchange is an established treatment option for several immune-mediated and neurological conditions. It is most commonly used when circulating antibodies, immune complexes, or inflammatory mediators play a significant role in disease activity. By reducing the concentration of these substances, plasma exchange can help modify disease progression when used alongside appropriate medical therapies.
Clinical specialties that frequently utilize therapeutic plasmapheresis include neurology, immunology, nephrology, and hematology. In neurology, plasma exchange is often considered in conditions where autoimmune processes affect the nervous system. In immunology and hematology, the procedure may be used to address disorders involving abnormal immune responses or plasma-related blood abnormalities.
Conditions that may involve plasma exchange as part of care include autoimmune encephalitis, myasthenia gravis, select vasculitic disorders, and certain kidney or blood-related diseases. In many cases, plasma exchange is not a standalone treatment but part of a coordinated care plan that may include medication, monitoring, and supportive therapies.
Treatment frequency and duration vary based on diagnosis, disease severity, and individual response. Some patients may receive a limited number of sessions during acute illness, while others may require repeated treatments over time. Physician assessment and ongoing evaluation guide these decisions to ensure appropriateness and safety.
Plasma Exchange in Longevity and Preventive Care
Interest in plasma-based therapies has expanded beyond acute medical treatment into preventive and longevity-focused care. As individuals age, changes in plasma composition can occur, including shifts in inflammatory markers, immune signaling proteins, and metabolic byproducts. These changes are an active area of medical and scientific research, particularly in relation to how circulating plasma factors influence tissue repair, immune balance, and systemic resilience.
From an educational perspective, it is important to distinguish between established medical use and emerging wellness applications. In preventive care settings, plasma-based services are explored as part of a broader strategy that may include lifestyle modification, metabolic optimization, and physician-guided monitoring. Plasma therapies in this context are not intended to replace conventional medical treatment but rather to support informed, proactive health planning.
The therapy involves the intravenous administration of donor plasma following consultation, screening, and physician approval. Patients considering this option often seek a better understanding of how plasma composition may influence inflammatory balance, recovery capacity, and overall physiological signaling.
Patients report a range of experiences following plasma-based therapies, which may include perceived changes in energy consistency, mental clarity, or general well-being. These responses vary by individual and depend on factors such as baseline health, treatment frequency, and concurrent medical care. For this reason, educational discussions emphasize realistic expectations, conservative scheduling, and ongoing clinical oversight.
Longevity-focused plasma services are typically discussed with adults who prioritize long-term health planning and structured medical guidance. Candidacy for Young Plasma therapy is confirmed through consultation, laboratory review, and medical screening. This process supports informed decision-making and helps patients understand how plasma-based therapies may fit within a comprehensive wellness approach.
Step-by-Step Plasma Exchange Procedure
A therapeutic plasma exchange session begins with a medical evaluation. Physicians review medical history, medications, and laboratory results to confirm suitability for treatment. This assessment helps identify potential risks and ensures that the procedure aligns with patient health status. Patients may also discuss prior experiences with intravenous therapies, sensitivity to fluids, or concerns about comfort during treatment.
On the day of treatment, the patient is positioned comfortably in a clinical setting designed to support monitoring and ease of access. Baseline vital signs are recorded, including blood pressure, heart rate, and oxygen saturation. An intravenous line is placed, typically in the arm, and secured to allow consistent blood flow throughout the procedure.
Blood is then processed through a plasmapheresis machine that separates plasma while returning red and white blood cells to circulation. The equipment operates continuously, allowing plasma removal and replacement to occur simultaneously. Clinical staff remain present to observe the patient, adjust flow rates if needed, and respond to any sensations such as mild chills, tingling, or pressure at the IV site.
Replacement fluids are infused as plasma is removed to maintain blood volume and electrolyte balance. Depending on the treatment plan, these fluids may include saline, albumin, or donor plasma selected by the physician. The procedure typically lasts one to three hours, depending on clinical goals and the volume of plasma exchanged.
During and after treatment, patients can generally expect the following steps:
● Ongoing monitoring of vital signs and comfort throughout the session
● Periodic assessment of fluid balance and circulation
● Brief observation after completion to confirm stability before discharge
● Review of post-procedure guidance related to hydration, activity level, and follow-up care
After completion, patients are observed briefly before discharge and provided with clear post-procedure guidance. Follow-up recommendations are based on individual response and physician assessment, supporting continuity of care and patient safety.
Safety Standards and Patient Care

Safety protocols are central to plasma exchange and plasma-based therapies. Clinics follow established therapeutic apheresis guidelines, including sterile technique, equipment maintenance, and standardized procedures.
Pre-Treatment Screening
Prior to plasma exchange, patients undergo screening that includes review of medical history, current conditions, medications, and laboratory values. This step allows clinicians to assess appropriateness and reduce potential risks.
Monitoring and Recovery
During treatment, clinical staff monitor vital signs, blood parameters, and patient comfort. After the procedure, patients receive guidance related to hydration, activity, and recovery. Follow-up is recommended based on individual treatment plans and physician advice.
Plasma Exchange Clinics and Available Services
Plasma exchange services are delivered in specialized clinical environments by trained medical professionals. Clinics offering these services are staffed by physicians, nurses, and apheresis specialists with experience in plasma separation and patient monitoring.
At Thrive Medicine Clinic, services may include therapeutic plasma exchange for medical indications and plasma-based infusion therapies offered within wellness programs. Each service follows defined clinical protocols and emphasizes individualized assessment and oversight.
Planning Your Consultation and Next Steps
Learning about plasma exchange or plasma-based therapies begins with a consultation. During this visit, patients discuss medical history, health goals, and available options with a qualified medical team.
At Thrive Medicine Clinic, consultations allow patients to receive education about therapeutic plasma exchange concepts as well as plasma infusion services such as Young Plasma. This process supports informed decision-making and helps determine whether a given service is appropriate based on screening results and physician guidance.
