Peri Menopause Weight Gain: Understanding Changes and Finding Support That Works
Many women entering midlife notice that their bodies begin to change in ways that feel unfamiliar. Weight gain, especially around the midsection, can feel sudden and frustrating, even when healthy habits remain the same. If you are noticing these shifts, you are not alone. Hormonal fluctuations, aging, and daily stress often combine to create a pattern known as peri menopause weight gain, a concern many of my patients bring to their visits. As a physician at Thrive Medicine Clinic in Houston Heights, my goal is to help you understand why these changes happen and what you can do to feel more comfortable and in control of your health. With the right mix of guidance, lifestyle adjustments, and medical support, meaningful progress is possible.
Understanding Why Weight Gain Happens During Peri Menopause
As women enter perimenopause, the body undergoes a transition that affects metabolism, fat distribution, mood, sleep, and energy. These changes often begin several years before the final menstrual period. During this stage, weight gain becomes more common, and many women notice an increase of a few pounds even without altering their diet. This shift is part of a natural response to fluctuating hormones and age-related metabolic changes.
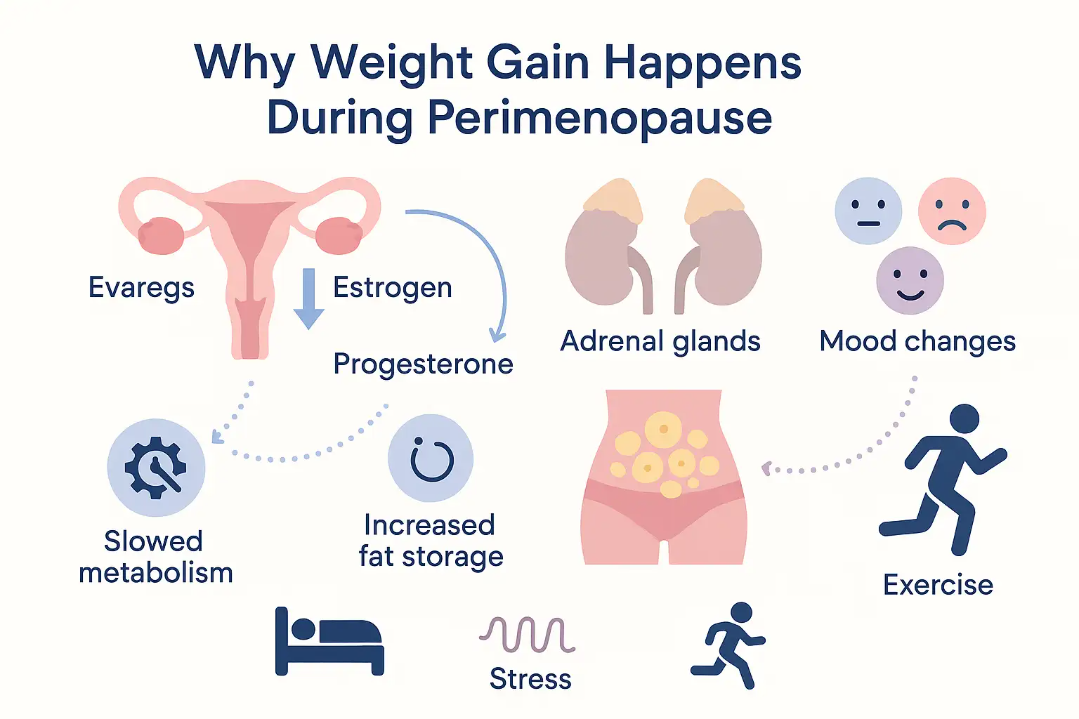
Estrogen plays a significant role in regulating where the body stores fat. When estrogen levels begin to decline, the body becomes more prone to holding weight around the abdomen. This shift is why many women describe feeling thicker through the waist or noticing a fuller midsection that resists traditional diet and exercise approaches. At the same time, progesterone levels vary, which can influence appetite, water retention, and mood. These fluctuations create the groundwork for changes in weight and shape.
Age also influences how the body handles calories. As metabolism slows, the body burns fewer calories at rest, which means even familiar eating habits may contribute to weight gain. Lean muscle mass naturally decreases with age unless resistance training or strength-based activities are part of a weekly routine. Less muscle leads to slower metabolic activity, which can make weight gain feel almost automatic.
Finally, daily stress plays a large role. Elevated stress levels increase cortisol, a hormone that encourages the body to store fat, particularly in the belly area. Many women in perimenopause also experience heightened stress due to life demands, career responsibilities, family transitions, and sleep changes. All of these factors combine to create an environment where weight gain becomes more likely.
Understanding these contributors helps you approach your health with clarity and self-compassion. What you are experiencing is not a personal failure. It is a physiological response to a shift in hormones, metabolism, and daily demands.
Why Belly Fat Becomes More Noticeable During Midlife
One of the most common concerns I hear from patients is a growing belly that seems to appear without warning. Even women who have maintained consistent routines for years may find that their midsection changes shape during perimenopause. This is often referred to as the “menopause belly,” and it develops due to a combination of hormonal shifts, age-related changes, and lifestyle factors that influence fat distribution.
When estrogen levels decrease, fat storage shifts from the hips and thighs toward the abdomen. This redistribution happens even in women who have always carried weight in other areas. Hormonal balance plays a strong role in determining where the body prefers to store energy, and midlife represents a turning point in that pattern.
Sleep disturbances also contribute. Many women experience night sweats, early waking, or difficulty staying asleep during perimenopause. Research shows that poor sleep is closely linked with higher levels of hunger hormones and increased cravings for high-calorie foods. When sleep is disrupted, the body has difficulty regulating metabolism, which encourages fat storage.
Stress amplifies this pattern. Elevated cortisol signals the body to store fat centrally, partly as a protective response. During perimenopause, women may face increased stress at work, changes in family dynamics, or health challenges, which can intensify this biological response.
Reduced activity levels can also play a role. Even small decreases in daily movement or exercise frequency can influence midsection weight. As metabolism slows with age, the body requires more intentional activity to maintain previous levels of calorie burn.
It is important to remember that the presence of belly fat during perimenopause is not solely cosmetic. Central fat is associated with metabolic changes, blood sugar fluctuations, and increased inflammation. Recognizing these changes early allows you to take targeted steps that support both appearance and long-term health.
Practical Strategies to Support Healthy Menopause Weight Management
Managing weight during perimenopause requires a thoughtful approach that works with your changing physiology. The strategies that helped in your twenties or thirties may not produce the same results today, and that is completely normal. What matters now is focusing on choices that support metabolism, promote balance, and fit within your daily life.
A balanced diet is a helpful foundation. Emphasizing whole foods, lean proteins, vegetables, fruits, and whole grains supports stable blood sugar and consistent energy. Increasing fiber intake can improve digestion, reduce cravings, and promote fullness. Foods like beans, lentils, oats, leafy greens, and berries are excellent sources of natural fiber and can support weight management with minimal restriction.
Regular exercise is equally important. A combination of strength training and moderate aerobic activity helps preserve muscle mass and supports a healthy metabolism. Strength training encourages the body to maintain muscle, which burns more calories at rest. Even two or three sessions per week can make a meaningful difference.
Sleep deserves special attention. Prioritizing a relaxing routine, maintaining a consistent bedtime, and reducing screen time before sleep can help improve the quality of rest. When sleep improves, metabolism, appetite regulation, and mood often improve as well.
Stress management is another essential pillar. Practices such as deep breathing, meditation, walking, stretching, or yoga can lower cortisol and help the body shift out of a chronic stress state. These techniques are not about perfection, but about creating space for balance in your day.
Magnesium may play a supportive role as well. Some women find that magnesium helps with relaxation, sleep, and muscle function. If supplementation is appropriate, we can discuss the right form and dosage based on your needs.
While these strategies do not replace medical treatment when needed, they provide a strong foundation for wellness and weight balance during perimenopause.
When Diet and Exercise Are Not Enough: Medical Options That Can Help
Despite doing everything right, many women still find themselves struggling with stubborn weight during perimenopause. This resistance can feel discouraging, but it is common and understandable. Hormonal changes, reduced muscle mass, metabolic shifts, and increased stress can create a perfect storm where progress feels slow or nonexistent.
When these challenges persist, medical support can provide a path forward. At Thrive Medicine Clinic, we offer personalized treatment plans that help women overcome weight plateaus and regain confidence in their bodies. Tirzepatide is one of the medications we may discuss when lifestyle changes alone are not producing the results you want. It works on multiple systems in the body to support appetite control, improve insulin response, and encourage weight loss. For many women, it provides a much-needed reset that allows the body to respond differently to nutrition and activity.
Before beginning any medication, we start with a detailed assessment. This includes reviewing your medical history, hormone patterns, sleep habits, daily routines, and goals. We take a whole-person approach to understanding your needs. Tirzepatide is not the right choice for everyone, but for women dealing with resistant weight gain, it can provide meaningful support.
Your treatment plan may include nutritional guidance, activity recommendations, supplement strategies, and ongoing follow-up to help you track changes. The goal is to provide clear direction, consistent support, and a partnership that helps you feel empowered during an important stage of life.
Partnering With Thrive Medicine Clinic for Personalized Support
Navigating perimenopause does not have to be overwhelming. With the right tools, guidance, and medical support, you can feel healthier, more energized, and more confident in your body. At Thrive Medicine Clinic in Houston Heights, we partner with women to create personalized plans that address the full picture of perimenopause health.
If you are noticing changes in your weight, energy, or overall well-being, schedule a consultation with our clinic. Together, we can determine what is driving your symptoms and build a plan that supports your goals.
You deserve clear answers, compassionate care, and practical solutions that help you feel your best during this transition.
